Look better. Feel better. Fountain of youth promises are making med spas one of the fastest-growing segments in healthcare. Botox injections, laser hair removal, IV hydration and therapy, medical weight loss, and hormone therapy seem to be available on every corner.
But most med spas are not compliant with Texas law. Either they are formed as the wrong entity type, they lack proper oversight and ownership, or all the above.
The consequences can be significant for everyone involved.
Med spa owners face potential civil and criminal liability for the unauthorized practice of medicine. Physicians associated with those med spas could find themselves subject to disciplinary action from the Texas Medical Board. And patients are caught in the middle.
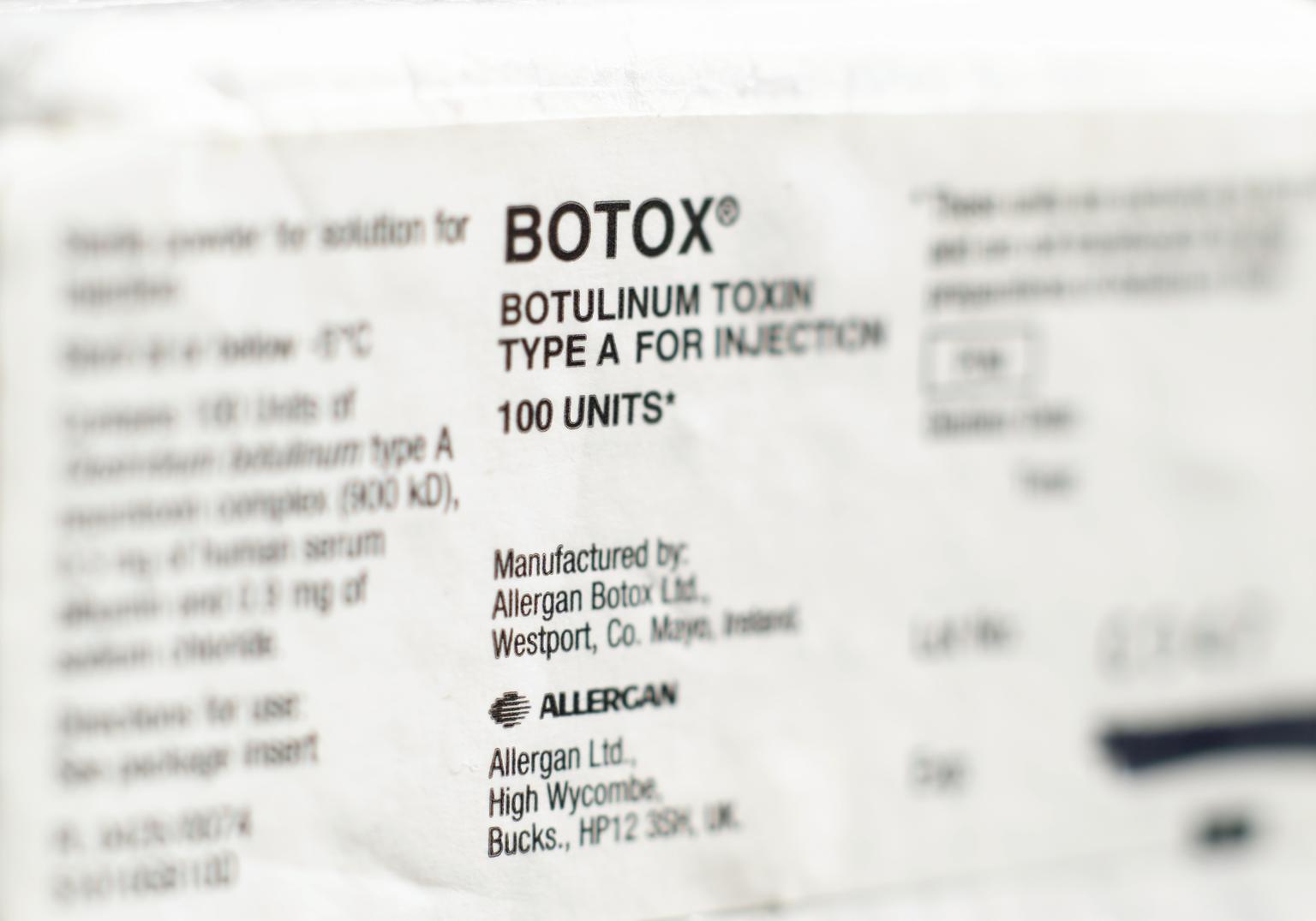
The “med” in med spa stands for medical because many of the services they provide are medical in nature. Botox, Disport, Juvederm, and Kybella injections, microneedling, chemical peels, laser hair removal, dermaplaning, and CoolSculpting are considered “nonsurgical medical cosmetic procedures” by the Texas Medical Board.
IV hydration and therapy, platelet-rich plasma injections, medical weight loss injections, and hormone therapy are also medical services. If a procedure involves injecting a patient intravenously or subcutaneously, it is probably a medical procedure.
Before any medical procedure, a physician or midlevel provider (like a physician assistant or nurse practitioner) must perform a good faith exam, establish a medically appropriate treatment plan, and document everything in a medical record.
Midlevel providers must be supervised by a physician under a Prescriptive Authority Agreement. The physician must review a sample of the charts regularly and generally be available to the midlevel if they have questions.
This does not happen in many med spas.
Then there’s the business side. The practice of medicine in Texas is regulated by the Texas Medical Practice Act, the Texas Medical Board, and administrative rules. Because med spas provide medical services to the public, they must comply with all these rules just like any other medical practice.
Med spas must be formed as an acceptable legal entity type. In Texas, medical practices are limited to professional associations (PAs), professional limited liability companies (PLLCs), and general partnerships with other licensed physicians. Many med spas are incorrectly formed as corporations or regular LLCs.
This is not just a technical problem. It leads to improper ownership. Medical entities, like med spas, cannot be owned by non-physicians. They must be owned by persons licensed to practice medicine in Texas.
There is a lot of information on the Internet, much of which is incomplete or wrong.
Texas is a “Corporate Practice of Medicine” state, which means that physicians cannot be employed to provide medical services by companies not owned by licensed physicians. In practical terms, a non-physician cannot start a company and then hire a physician to provide medical services to patients of that company. With very few exceptions, medical services can only be provided through professional entities owned by physicians.
These same prohibitions apply to midlevel providers like Physician Assistants and Nurse Practitioners. Physician Assistants can co-own a medical practice with a physician only if the physician controls a majority interest in the practice. Nurse Practitioners cannot own any percentage of a medical practice.
These are just a few of the compliance issues for Texas med spas. There are also in-office and website disclosure requirements, registration requirements, reporting requirements, and restrictions on the type of marketing or advertising the practice can engage in.
Patients are caught in the middle. Those injured at a non-compliant med spa may not know where to turn.
These types of complaints to the Texas Medical Board are growing at an alarming rate. If the non-compliant med spa has a Medical Director, the Board can discipline the physician for inappropriate supervision or unprofessional conduct. Physicians associated with non-compliant med spas are putting their medical licenses at risk.
For the unlicensed med spa owner, the Medical Board can shut down their business. In extreme cases, the unlicensed med spa owner could be charged with practicing medicine without a license. If the patient suffers a physical or psychological injury, the owner could be charged with a third-degree felony which carries jail time of two to ten years and a fine of $10,000.
If the patient hires an attorney to sue for malpractice, the med spa’s insurance company may deny coverage if the med spa was not formed or owned in compliance with Texas law.
Med spas are big business and growing rapidly. But with great reward comes great responsibility. Entrepreneurs owe it to themselves and patients to set up the med spa the right way, with the right supervision, and the right ownership.